The PODS ToolKit
This toolkit will support your organization and provide guidance for implementing PODS. From experience it is feasible to go live with a pilot group within 6 months.
Just follow our 4-step process:
Click on the section you want to review first.




Get Ready
The first step to implementing PODS is to gain an understanding of what PODS is, what your current discharge education processes are, potential barriers and facilitators, and how PODS can help you achieve your goals. While you work to get ready keep in mind that PODS can:
1. Organize and streamline the discharge process.
2. Create awareness and understanding through guidance and teaching.
3. Become an aid for patients to refer to at home.
blank
Understand PODS & Your Current Processes
PODS is a set of best practice guidelines to ensure patients and their families get relevant and actionable information that they need to manage their care at home after discharge. Each organization takes the guidelines of PODS and adapts the tool and process to meet the unique needs of their patients. Talk to patients and families, staff, and other stakeholders to understand the current state.
First, understand the problem:
- Are there gaps in patient understanding of their instructions or in the consistency of your discharge education process?
- Are you looking to improve any measures related to patient satisfaction or experience in transitions in care?
Second, understand your current process.
We suggest that you begin with reviewing the current practices for providing key information to patients and families.
- Who is giving instructions to patients? When? How?
- Do patients currently receive things to take home? What are they?
- How is technology used currently in this process?
- Is there common or repetitive information or tasks that can be removed or automated?
- Are their other initiatives that can be leveraged?
Understanding current practices can help you figure out how PODS will fit into your process with minimal impact to workload and allow you to minimize change management. Additionally, this process can help identify other wins in terms of improving the discharge process. When reviewing the current state think about:
- Content – information patients are being given
- Design – how is that information presented
- Process – who is currently teaching the discharge instructions
Create a Working Group
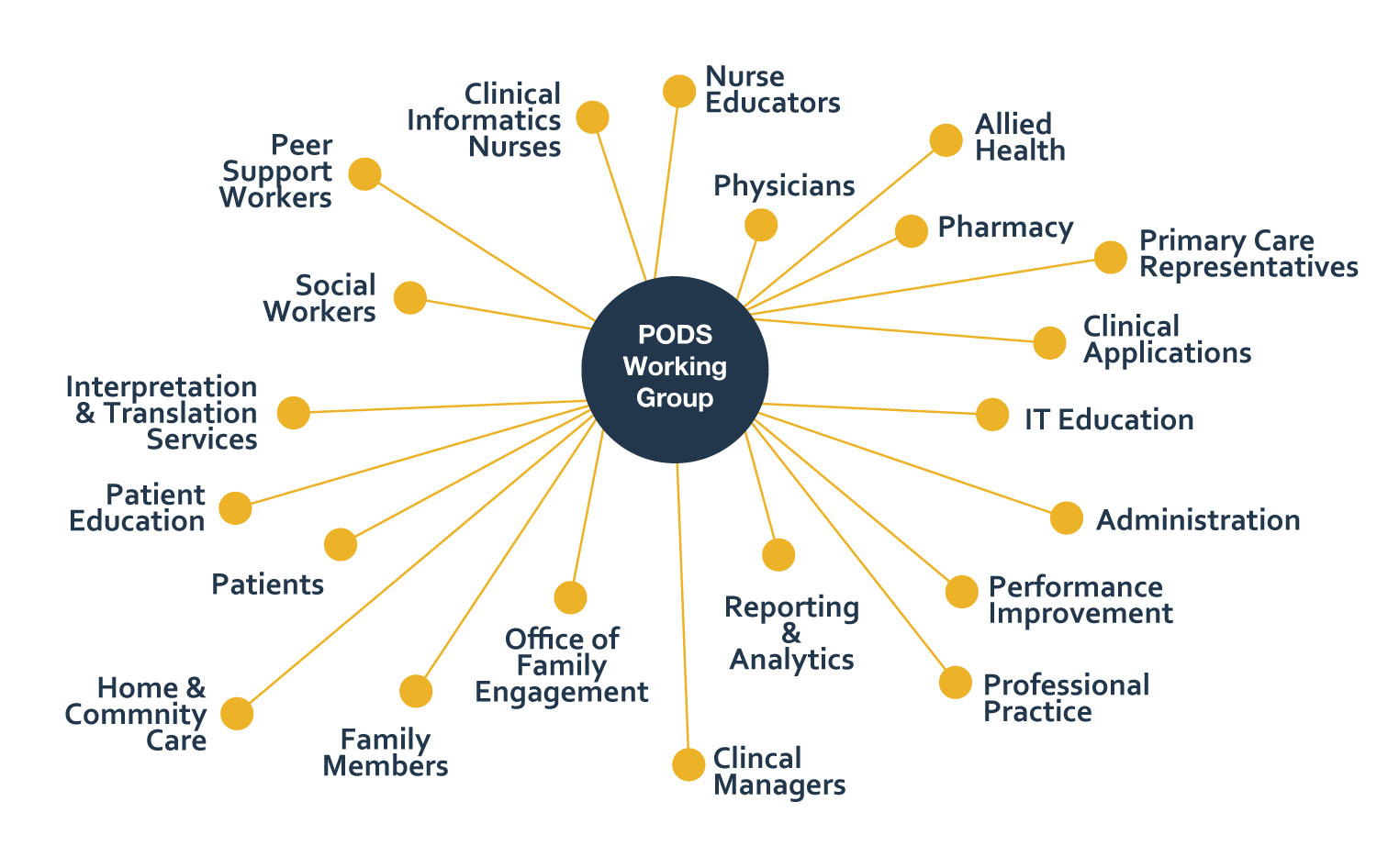
There are also many stakeholders affected by the process and instructions given to patients at discharge. Create a working group with a mix of stakeholders that includes patients and families. Although PODS was co-created together with many patients and families, when you are adapting it to meet the needs of your local population and processes, it is valuable to include patients and families from the outset and throughout the project.
Barriers & Facilitators
Keep in mind organizational barriers and facilitators early on in order to plan ahead and employ strategies to minimize barriers and ensure success.
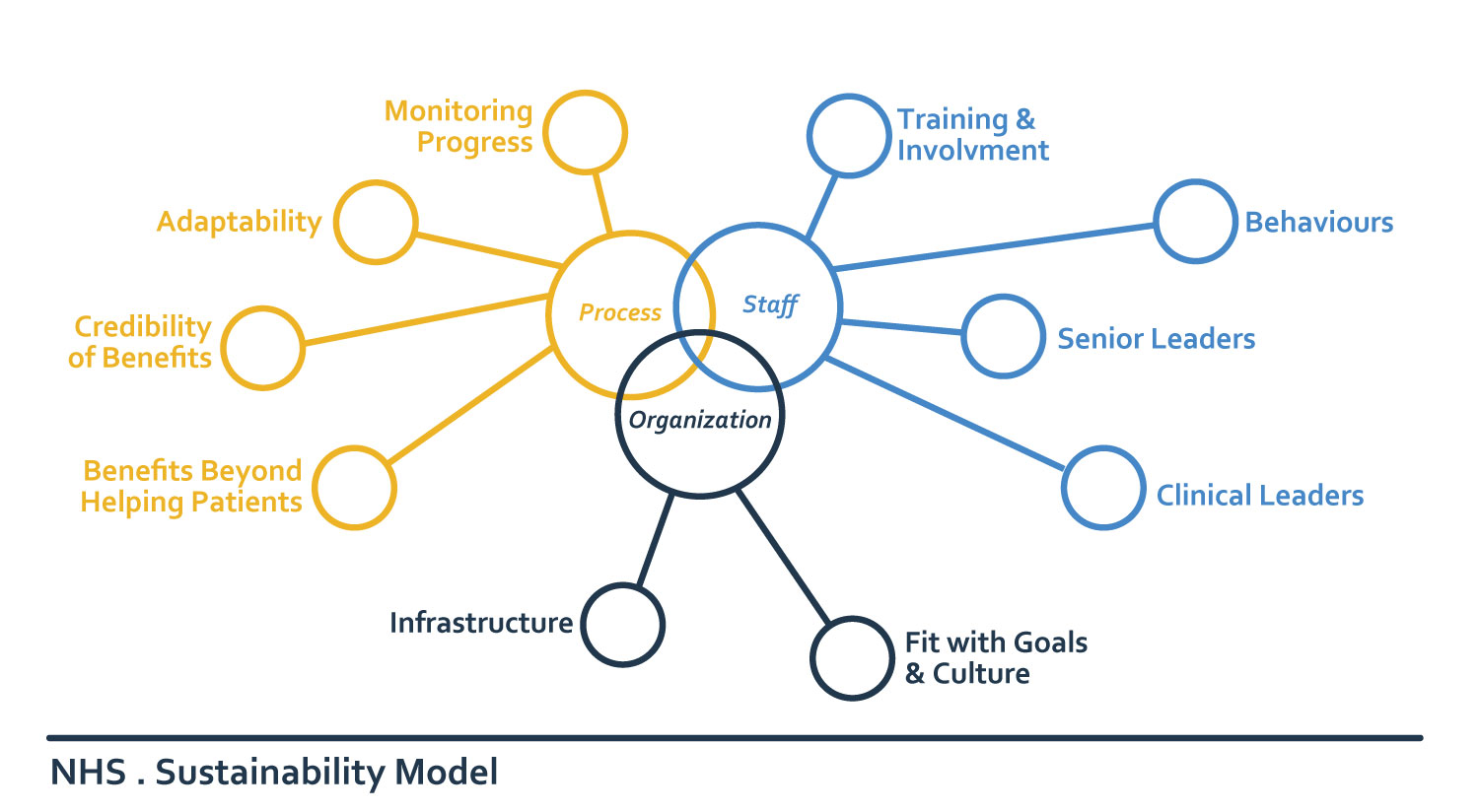
Thinking about sustainability early on helps with success in the long run. The NHS sustainability model outlines areas related to the process of implementing an intervention, staff support, and organizational factors that contribute to sustainability.
In our PODS work to date, the following barriers and facilitators have been highlighted:
Barriers |
Facilitators |
|---|---|
| Competing priorities and a shortage of time and resources. | 1) Champions and support at clinical and executive levels.
2) Culture that values patient experience, where other initiatives can be leveraged. |
| Staff acceptance when absent is a barrier and when present is a facilitator. | 1) Involve patients and families throughout and focus on their needs.
2) Include frontline staff in PDSA cycles. |
| Poor design that does not integrate into current workflow.
Complex team dynamics, high turnover, and complicated discharges. |
1) Spend time early on understanding current state. Use PODS to streamline the process and integrate it into workflow.
2) Connect with others who have implemented PODS with similar workflows and patient groups. |
| IT delays and electronic charting that confines what can be included and how it looks. | 1) Engage your IT department early.
2) Focus on the benefits of using an electronic tool. |
Design & Adapt
Your working group is now ready to begin designing and adapting the PODS. Work together with your staff and patients to figure out how to take the PODS best practices and adapt them so they meet the needs of your patients and families and staff. In addition to the best practices, you can use our PODS template as it is or as a starting point for your PODS form. When designing your PODS, think about the three main components of using PODS:
1. Content: What information to include.
2. Design: How the form is created and looks.
3. Process: How the information is given to the patient & family.
blank
Content
Think about the important information included in a PODS form. Is there anything you want to change or add? Some hospitals change wording in the template to reflect the nuances of their patient population.
Some examples of how PODS has been adjusted:
- Hospitals serving a population with mental health conditions, have changed the “Changes to my routine” section to “My goals and community help to reach them” and the “Where to go for more information” section to “My supports after discharge”.
- Many rehab hospitals have expanded the “Changes to my routine” section to list out activities of daily living with checkboxes noting whether the patient needs help for each task.
- Many hospitals have added checklists of reminders.
There is a trade-off between customization and standardization. For conditions with many standard instructions, you can pre-populate the PODS with content for that specific condition.
Another consideration is how to incorporate the “Medications I need to take” section. Some hospitals leave that separate and include a checkbox on the PODS form to ensure they go through the medication list with the patient. Others include a patient-friendly medication list.
Design
Think about how your PODS will look. This is especially difficult and important when implementing within an electronic system. Do your best to use clear headings and large font. If you can, allow for translation of the headings into common languages spoken by your patients. Other design considerations might be:
- Using automation and dropboxes to minimize clicks and typing.
- Using checkboxes to make sure important information is included like medications and whether appointments have been booked.
- Including as many icons as possible (for section headings, phone numbers, etc).
- Making space for the patient to take notes.
- Consider printing the PODS on coloured paper so that it is easy for patients to identify when they are at home.
About half of the hospitals who implement PODS use a paper form and half build it into their electronic systems. We have found that although it is completely feasible to build it into the electronic system and the build itself does not take long, there is often a queue of IT priorities. If you are planning on implementing electronically, connect with IT early.
Process
Use PODS to support those providing teaching to patients and families. It is an especially valuable tool to support the use of teach back, a technique where the provider asks the patient and family to repeat back what they understood. For example, a provider might say “Can you explain what you would do if you start to feel short of breath? I want to make sure that I explained it clearly”
PODS has also been shown to improve staff confidence and consistency in providing discharge instructions. Once it is embedded into your discharge processes, it does not add to workload and often saves time while ensuring a consistent process. To ensure your new process does not result in duplication of work, consider:
- Who fills out which section of the PODS when?
- Who goes over each section of the PODS with the patient and family and when?
- How will you be sure that the PODS has been completed and reviewed?
Some hospitals have a single provider own the PODS, some give it to the patient to fill out with the support of staff over the course of their hospital admission, and some share the responsibility with a multidisciplinary team. Most hospitals go through the PODS with the patient a day or so before discharge, but some start at admission, and others use the opportunity of a family/team meeting. There is no right or wrong way.
Train
Once everything is designed, it is time to train staff on the new processes and tools you will be using. By now you will have champions in the staff on board and you can engage them and your patient and family advisors in this portion as well. In addition to building it in to new staff training, you may want to send out some online resources and hold lunch and learns.
It can be helpful to start with a review of some of the current state results at your organization and the highlighted areas of opportunity, along with a review of the purposes of PODS and the evidence behind it to relay why you are implementing PODS.
blank
Content & Design
PODS is meant for the patient and family and should focus on information that is important for them when they go home. It should use plain language directed to the patient and not be too lengthy. If you are creating standardized PODS content, have it reviewed by patients and families.
- use common words
- avoid acronyms
- keep in mind what is relevant for the patient to act on
- be consistent with word use
- use analogies
- be thoughtful with mathematical concepts that may not have meaning to patients
A useful resource for providers to use when completing the PODS is this glossary of diagnoses described in patient-friendly language. Read more here.
Sample Translations:
Medical Jargon |
Plain Language |
|---|---|
| Hypertension | High blood pressure |
| S.O.B. | Shortness of breath or difficulty breathing |
| Contraception | Birth control |
| Feel for lumps about 5 to 6 millimeters in diameter | Feel for lumps about the size of a pea |
Process
PODS should be delivered in the presence of family using teach back, a conversation technique that asks patients to explain back in their own words what they understand. It is important to engage the patient and family in a conversation about their discharge and whether they have the help they will need at home and feel comfortable with their understanding of their discharge instructions. During the conversation, keep the following tips in mind:
- Greet your patient and introduce yourself
- Make eye contact
- Speak slowly and use plain language
- Solicit questions by asking “That was a lot of information, what questions do you still have?” Do not ask “Do you have any questions?” This often leads to a quick “no” even if they do have questions.
- When using teach back, use open-ended questions
Special considerations
There are patients with barriers to communication, cognitive impairment, limited health literacy, various disabilities, or financial barriers who may be at increased risk for not understanding or following their discharge instructions. Consider you patient population and what could be embedded into your PODS process that may help.
- Ask patients about their home life and whether they are comfortable with the follow up instructions you are providing
- Involve friends or family when providing instructions
- Work with your interprofessional team – for example, a speech language pathologist may identify strategies to help with communication and social workers may know of community resources that would benefit the patient and family
- Ask patients if they want to put on their glasses or hearing aid or use their phone to record the conversation
- Use services available to you such as a professional interpreter if their language preference is not English
- Ask about their drug coverage and ability to go to follow up appointments and consider prescribing generic versions that may be less costly, prioritizing certain follow up appointments for them, or finding health services that are closer to home
Look in the resources section for more detailed tip sheets when using PODS with various vulnerable populations.
Launch
You are now set to implement PODS! Get it out there and start using it.
As PODS is a quality improvement initiative, it will be an iterative process where you evaluate and refine the process as you go. As before, it is important to get input from stakeholders during the iterative process, especially patients and frontline staff engaging in the PODS process. Patient and families – to make sure it is meeting their needs. Frontline staff – to make sure it integrates into the day-to-day workflow.
blank
Promotion
Promote and get people excited about PODS.
In general, this is easy because PODS is exciting and it is all about the patient and family. That being said, some organizations that have implemented PODS have been very creative, posting on social media, creating t-shirts for PODS champions, etc. We have created some promotional materials that may be helpful to you during this phase.
Evaluation
Think about tracking and evaluation. Consider the measures already used to collect data at your hospital that may be relevant to PODS. For example, there are specific questions in the CIHI Canadian Patient Engagement Survey (CPES) that are relevant to discharge. PODS is likely to improve these measures:
- CPES Q19: During this hospital stay, did doctors, nurses or other staff talk to you about whether you would have the help you needed when you left hospital?
- CPES Q20: During this hospital stay, did you get information in writing about what symptoms or health problems to look out for after you left the hospital?
- CPES Q37: Before you left the hospital, did you have a clear understanding about all of your prescribed medications, including those you were taking before your hospital stay?
- CPES Q38: Did you receive enough information from hospital staff about what to do if you were worried about your condition or treatment after you left the hospital?
While you are implementing, keep track of how well the implementation is going.
- Are PODS being given consistently?
- How is the quality of the content and process?
You can track the percentage of patients who are given a PODS and do occasional audits to check on quality and increase your training efforts if needed. It is also useful to consult with or survey patients, families and staff to see how things are going and what improvements may be needed.
Quality Improvement
After you go live with PODS, as with any QI initiative, there will be things that didn’t work. PDSA cycles, daily or weekly huddles, and some change management will help. Many hospitals have experience with QI and will have learned from their previous projects what works for them. If you are looking for helpful tools at this stage, we recommend the set of QI tools created by Health Quality Ontario:
PODS by OpenLab is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License