PODS In Practice – Creating Patient Oriented Medication Tools

co-design session ~ 2019
Find templates of the tools described on this page on the resources page, in the Design and Adapt section: here
The process of being discharged from the hospital can be one of mixed feelings for many patients and families. Our previous work on the Patient Oriented Discharge Summaries (PODS) project highlighted that medication information is an area where having clear communication and education could not only ease patient anxiety on discharge, but provide valuable information to support self-care at home.
While in the hospital, healthcare providers take care of preparing and administering all medications. This is a necessary part of care, patients can be monitored as medications are changed to optimize their overall health. Problems begin to arise as these responsibilities are transitioned to patients and their family members. Once at home, it can be overwhelming. Patients are often given a list of new and/or changed medications and for some, the list when leaving the hospital looks very different from the list when they entered. The unfortunate reality is that the time spent with patients and families at discharge going over their new medication list is limited at best, a sentiment conveyed to us during research and codesign by patients, families, and pharmacists. This often leaves patients and families with many unanswered questions, such as how the new medications fit into their routine, what they should do with their old medications, and sometimes even where to get their new medications.
Fortunately, solutions are simple as the majority of issues result from gaps in communication:
- Have systems in place to provide structured and consistent information about medications to patients and families
- Involve patients and families in the creation of their medication routine while they are still in hospital
These solutions ensure patients and families can leave the hospital better equipped with information on not only how to access their medication, but how to take it and where they can go if they have questions.
During the Hospital Stay
Patients and families that we have engaged, reported that they are rarely involved in creating medication routines while in hospital. Ultimately, this leads to issues when they get home.
Opening up lines of communication around medication is not a need reported solely by family members—pharmacists who consult with patients in the community agree that spending time before discharge to establish a routine could help greatly with medication adherence.
“Nurses help administer the meds at bedside, they know to crush the meds, but they don’t tell the family, and when discharge happens, families are lost. Families feel that a lot of information given is driven by the healthcare provider, what they want to tell the patients, what they think is important.. but the patient’s needs are different. It should be open-ended for the family to identify problems they might have.”
– family
“We need to establish a routine before the hospital discharge,.., Figure out what her day is like and what her needs are at each point…And align her home and hospital routines. Another thing is it needs to involve education pieces when she’s at the hospital.”
– pharmacist
“Discharge is the most stressful time and routines with medications should be done in the hospital and practiced before discharge…Discharge is not a one- time moment.”
– patient
Transitions simply are not binary and we cannot treat them as such. In order to redefine how we equip patients as they are sent home, we need to stop thinking about the moment of discharge and start talking about the entire hospital visit as a process.
Poor Communication in Hospital Carries Over Once the Patient is Home
Imagine returning home from the hospital, opening up your package of medications that you picked up from the pharmacy only to realize that what was printed by the pharmacy was completely different from what you were told at the hospital. This was the reality for one family who described the anxiety they felt around taking medications. What’s worse was that, despite their best efforts, they couldn’t get in touch with the doctor.
“And there was this injection for blood thinners on the list and she said mom was supposed to be getting it at home and we haven’t heard anything about it. So I don’t know if it is accurate or not.”
– family
Many of these communication problems are made worse for individuals with language or learning barriers. One patient with language barriers told us that he doesn’t like to interrupt his doctor to ask questions about his medications. Instead, he writes down the sounds of the words that the doctor says and uses Google to look them up later.
“I look them up or figure them out. I’m trying. Like if the medications are not the same as the brand names are right. And when I go to the internet and look them up. And that takes a lot of time and that’s a nuisance.”
– patient
Other patients and families told us about how they have difficulty understanding the medication lists provided at the hospital. Some look up the medications on the internet and others go to their community pharmacy for clarification.
When given the time to speak with a pharmacist and ask questions, many patients find that they are better equipped to take their medications at home. Unfortunately, the problem still remains: can we create a system that supports patients in getting this information?
Creating Patient Oriented Medication Tools

Throughout our work designing PODS, and learning from its implementation and other research, medication information remained an opportunity where tools could be created to support healthcare providers, patients, and families in making sure understandable and useful information is provided to patients and families when they transition from hospital to home.
We used a process where we designed with high-need users, specifically patients and families with complex medication and communication needs: those with language barriers, physical disabilities, and developmental disabilities. Our process involved two phases with integrated engagement of hospital and community pharmacists and patients and families:
(1) Exploring the information needs related to medications when patients transition from hospital to home, and
(2) Designing tools to support providing the information needed.
In order to explore the space, we reviewed knowledge about medication information needs that arose during the co-design of PODS and subsequent work in implementation, evaluation, and research related to PODS. We also conducted a scan of popular medication management apps and conducted many interviews with patients, families, pharmacists, and physicians in the hospital and community. In order to begin designing tools, we synthesized what we had learned about medication information needs into case studies where key needs were highlighted and then held a collaborative engagement session with patients, families, and healthcare providers to define the needs related to content, design, and process. The defined needs were then used to create prototypes of tools that were taken to groups of patients, families, pharmacists, and physicians to be interrogated. Their feedback was used to refine the tools described here.
The Tools
We created three tools to support the communication and education of medication information for patients and families transitioning from hospital to home. Find and download the tools here.
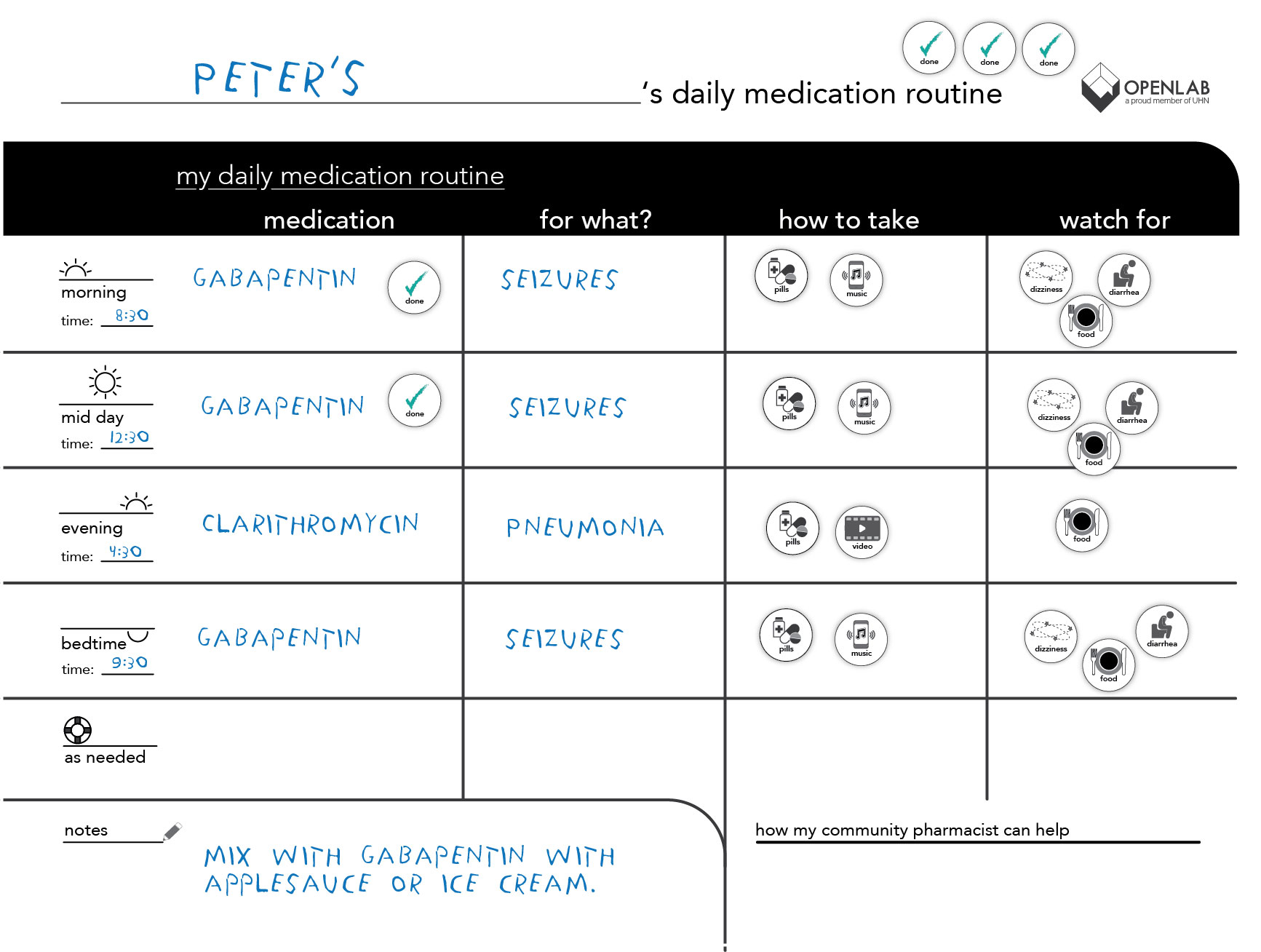
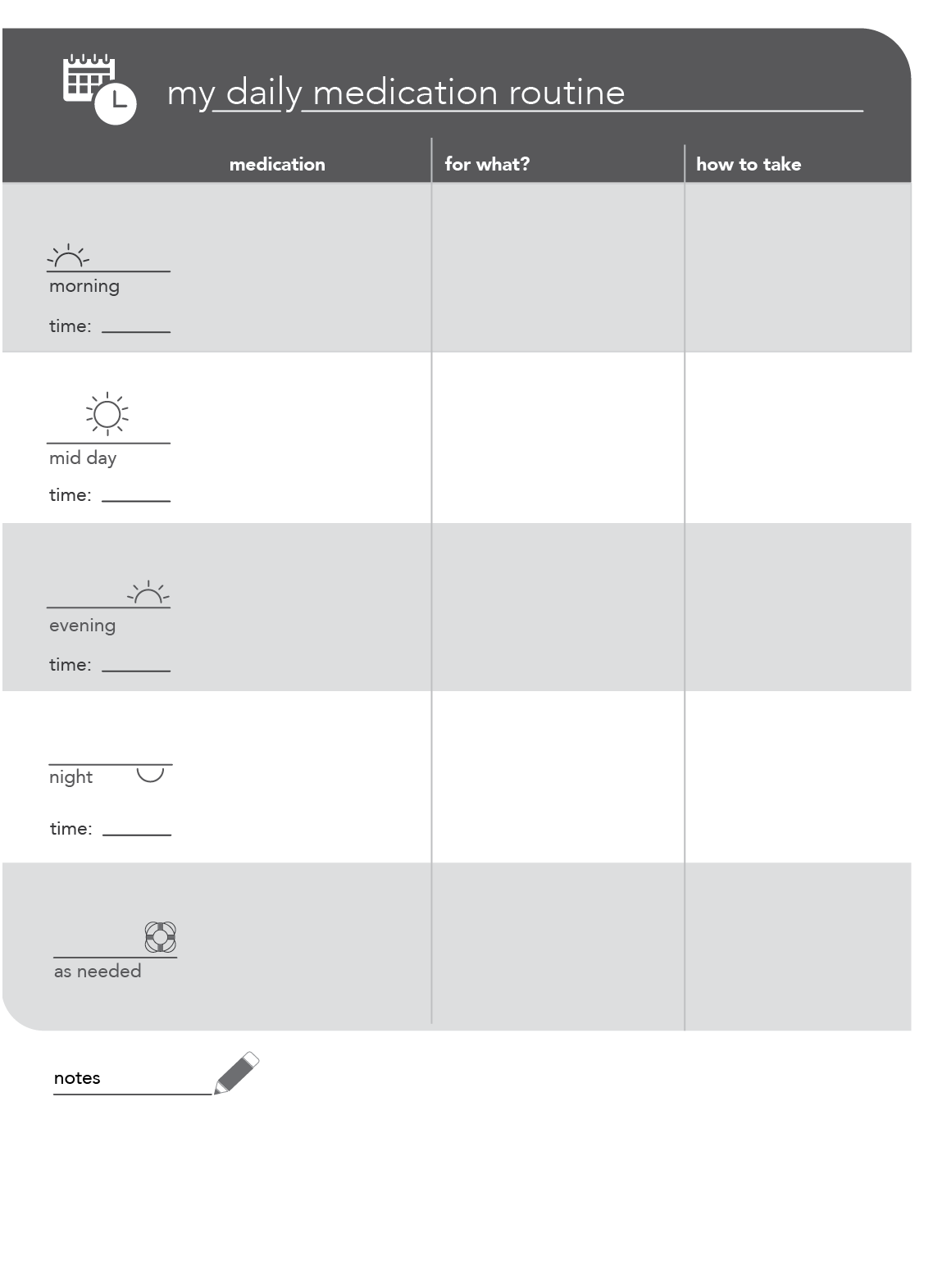
Medication Whiteboard. The Medication Whiteboard is meant to be used while in hospital. It involves the patient and family in creating their medication routine and starts communication and education early in the hospital stay. It comes with a set of magnetic tiles with icons that represent possible medications, reasons for taking medications, and tips on how to take them to support involvement of patients who have communication difficulties
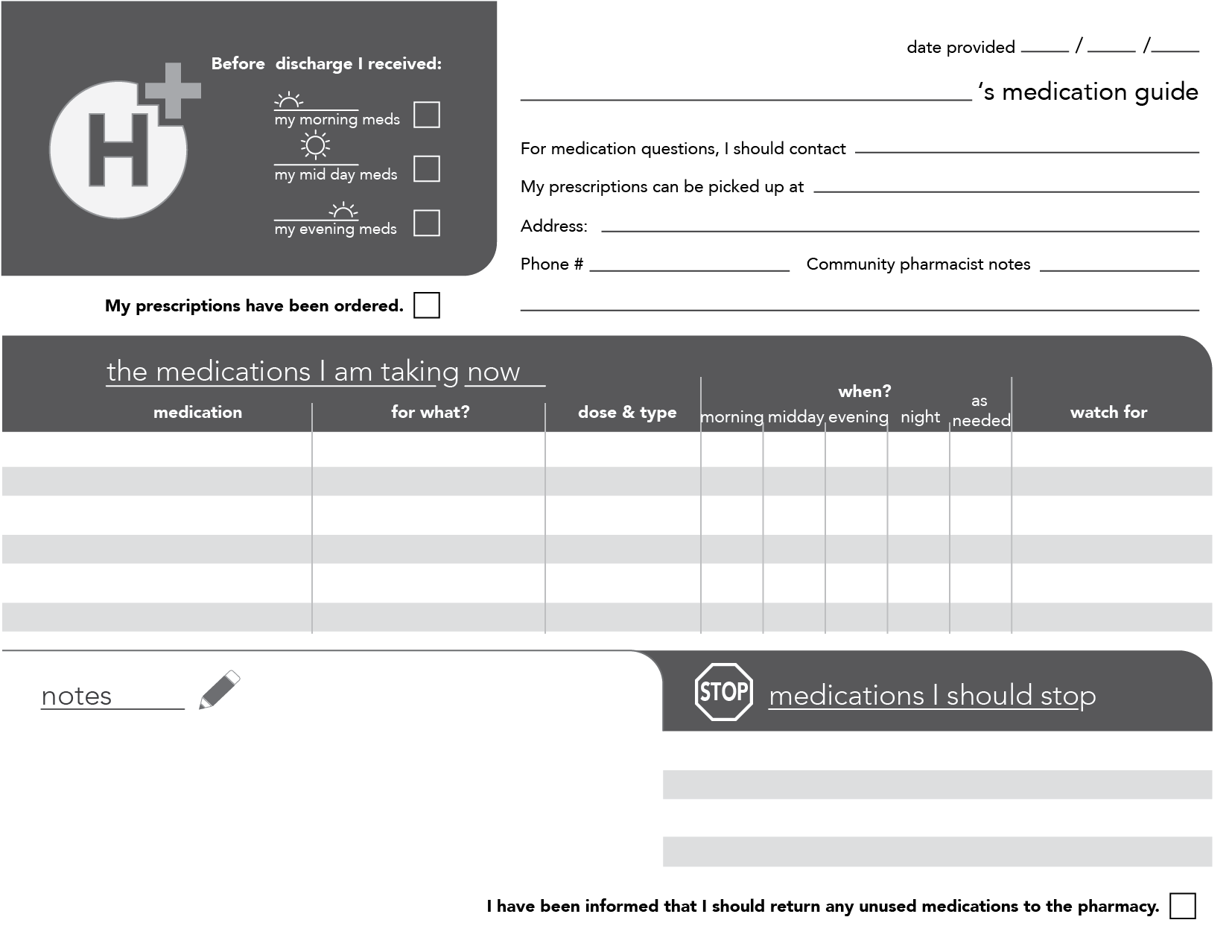
Patient Oriented Medication List. The List is meant to accompany a PODS. Using conversation and teach back, the healthcare provider can use the list to provide education about each medication the patient needs to take. The list also clearly communicates which medications to stop taking, information on how the community pharmacist can help, and who to call if they have questions about their medications.
Blister Pack Insert. This list reinforces the medication routine created using the whiteboard. It can be used on its own as a visual reminder of the medication routine and is designed to fit inside the inside cover of a blister pack.
If you want to learn more about how to use these tools, the tools as well as a complete best practice user guide can be found here. Hospitals are welcome to use the tools as is or take the guidelines and adapt them to fit the needs of their patients and processes.