PODS in Practice: Improving the Transition Experience at CAMH

PODS Team at CAMH
Back Row: Jaime Boccongelle, Gillian Saracino. Front Row: Dmytro Pavlov, Cara Mirabelli, Rachel Solomon, Jennifer Wilkie, Rita Desai
The clean, clinical halls of the Centre for Addiction and Mental Health’s (CAMH) inpatient clinics are teeming with life. Patients move in and out of the bright common area at the end of the long hall, where they socialize with other patients and the clamour of various activities can be heard floating throughout the ward. The long hospital hallway is lined with tall wooden doors, each one adorned with a hand drawn picture bearing each residents name – a warm touch for their temporary home. For each of these patients, their stay at CAMH will come to an end and they will be discharged from the hospital, marking the beginning of an incredibly vulnerable time for patients.
“Our patients get bombarded with a lot of information on discharge. Follow up appointments and things like that. They're often quite stressed at discharge.”
As Charlotte Rowell, a clinical social worker on the geriatric unit, explains, information overload is only one aspect of stress at discharge for patients: a changing environment, the effects of treatment, and the complexity of mental illness all intersect at this transition point. The interplay of these factors often makes it difficult for patients to retain the important discharge instructions they are given. At CAMH, ensuring that patients are equipped with appropriate discharge information has been identified as a high priority need. As Rachel Solomon, Executive Director of Performance Improvement at CAMH, explains,
“We looked at our patient experience results and saw that the thing that our patients were most upset about was not having the information they needed when they left the hospital, and that's consistent with what we'd seen in the evidence. Being a data-driven organization, we looked at what our patients were telling us and what the evidence told us and it came together. [We] said we needed to implement something like PODS and I was thrilled to see that at CAMH we actually implemented PODS across every inpatient unit.”
PODS is a set of guidelines and tools co-created with patients and families by OpenLab at the University Health Network to improve how information is communicated to patients when they transition out of the hospital. PODS was designed according to best practices by providers, caregivers, and patients, specifically hard-to-reach patient groups such as those with language barriers, mental health issues, and limited health literacy. Designing PODS with patients was important, not only to capture the diverse needs of different patient groups, but to empower patients that are often overlooked, a problem that Solomon says mental health and addiction patients constantly face.
“Individuals with mental health and addictions issues frequently are an afterthought within the health care system. People say ‘we'll build something for acute care and hope it works for mental health.’ [PODS] gave us the opportunity to be part of the same large group as everyone else and to look at it and adapt it for [our] population. There's such a gap within mental health and addictions that I think people were very excited to be part of a first wave and not a last thought in helping serve the patients that we have.”
PODS is designed to be modular. Solomon and her team at CAMH took the core PODS documents and engaged a diverse group of stakeholders, which included social workers, clinical pharmacists, physicians, and, of course, lots of patients. In addition to these internal stakeholders, the CAMH team engaged community agencies and family physicians in the implementation of PODS as well. For the CAMH patient population, this was vital as many rely on these community services on a regular basis. As Rowell says about her patients in the geriatric clinic,
“Especially with the long-term care homes, [when they] get the PODS ahead of time they can sort of see a quick summary of what happened.”
What this demonstrates is how valuable a tool like PODS can be for members of the care team that normally don’t receive documentation about a patients stay. Now that PODS is implemented, Solomon continues to receive feedback from these stakeholders about how PODS has helped improve their ability to provide care and services.
“We hear a lot of specific feedback from housing providers who have said to us that they now actually know in clear and simple information when their patients bring in or their clients bring in their PODS what has happened in the hospital."

PODS can be implemented in either a paper or electronic format. CAMH built an electronic version of the form into their Electronic Medical Record (EMR) system. As Solomons states, this decision was intentional,
“It was really important for us to make PODS electronic. In doing so, we were able to sustain this with not a lot of additional work for our clinicians.”
The need to find a solution that didn’t increase the workload at discharge came up during the engagement sessions with members of the care team. As a result, not only did they find a solution that maintained the integrity of internal workflows, but their EMR system can also seamlessly send PODS to any relevant community agencies via auto fax, further ensuring the continuity of care for patients being discharged.
In addition to ensuring that existing workflows were not disrupted, another key consideration when designing and implementing PODS at CAMH was keeping it simple for patients.
“PODS has been very useful for our patients that have cognitive impairments. We are seeing that this is a great tool for them so they remember follow ups or what happened during their admission.”
According to Rowell, this is a dramatic improvement from the previous discharge summary that was given to patients.
“We would give them a big discharge summary and that was really complicated for an everyday person to read. So we had a lot of missed appointments and people [were] confused as to what their medications were on discharge.”
Old discharge summaries were often filled with medical jargon and designed in a way that made them difficult to read. PODS is designed to use language that is patient-friendly, which greatly streamlines the communication of post-discharge information. As a result, social workers are empowered to be more goals focussed, highlighting that their care goes beyond overcoming the current crisis. As Kiera Marshall, a clinical social worker in the Mood and Anxiety Clinic describes,
“It outlines their goals, whereas I think oftentimes when we think of discharge planning we're thinking of what we think would be helpful for them. Instead, it's like, ‘what are your goals’ and trying to make sure that you're including specific information that may be relevant.”
Marshall goes on to describe how she handles discharge with her patients now that the PODS tool has been implemented:
“I find myself saying, which I never used to say before, ‘On the day of discharge I'm not going to be giving you any new information. I'm just going to be reviewing the stuff that we've sat down and talked about already.’ ”

In addition to streamlining communication to patients, PODS has become a nexus of collaboration for members of the care team at CAMH.
“As a pharmacist it really helped get me involved in the process at discharge,”
According to Noreen Jamal, a Clinical pharmacist at CAMH, the pre-PODS workflow for pharmacists did not have any cross-talk with that of physicians and social workers. Now Jamal can include the appropriate medication information in patient-friendly language and ensure that they are appropriately counselled in the clinic before leaving.
Clinical pharmacists like Jamal now have a medication table that is designed to clearly outline what medication a patient needs to take, when they need to take it, and the benefit it will bring them. It also outlines what the patient may experience while on this medication, ensuring that they are aware of any potential adverse effects. According to Rowell, the medication table is admired by more than just the patients:
“My favourite part of PODS is this beautiful medication calendar that it produces. It's super clear.”
Having an easy-to-understand medication calendar also means that patients and family members can go home and digest the information at their own pace instead of trying to understand it all at the clinic. This is especially important because if patients understand how a drug can benefit them, they are more likely to be compliant in taking it. She continues to say,
“It's really important that we do have to work as a team. There's certain parts that have to be done before we're able to do our part and before we're able to sign off on the PODS document. Your team does have to be very integrated.”
So what does the PODS process at CAMH look like? Well it can be broken down into four steps:
1) CAMH PODS is filled out through their EMR system. During a patients stay at CAMH, various members of the clinical team (Physicians, Recreational Therapists, Pharmacy, etc.) will enter information into their respective sections on the EMR, which includes a ‘Discharge Planning’ form.
2) The clinical social worker and/or nurses will create a PODS form on the EMR. Many of the PODS sections—Medications, Appointments, How I Might Feel and What To Do, and My Supports After Discharge auto populate from the discharge planning form. At this time, the social worker can engage any clinicians to input missing information and add any appointments that were not logged in the system.

3) When the PODS is completed on the EMR, a copy or copies are printed out as needed. If the patient has a family member or a caregiver, the patient will be asked to give consent to share their PODS with that person. In addition, family doctors or family health teams can request that a copy be faxed to them as necessary.
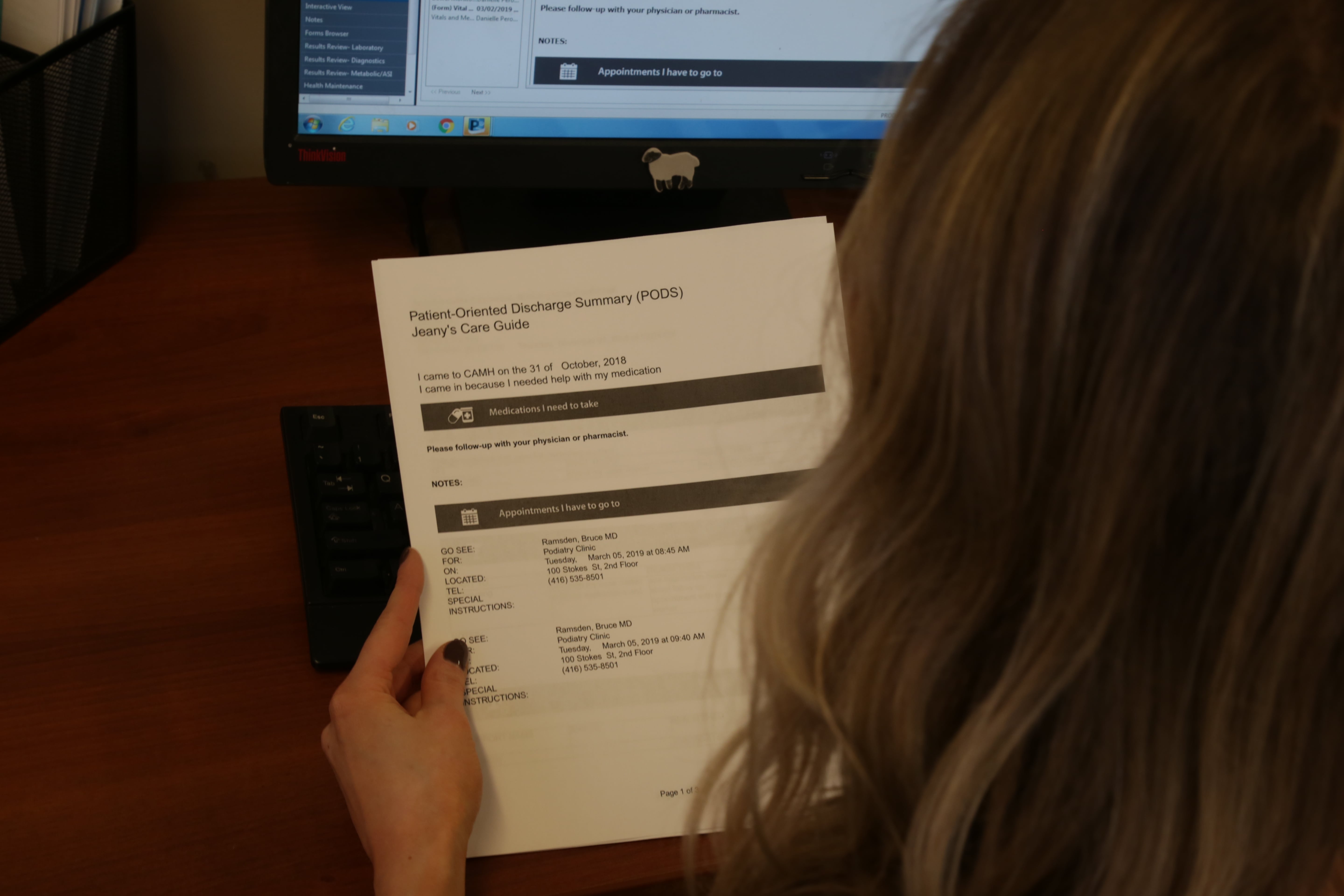
4) A copy of the PODS is taken to the patient’s bedside and reviewed with them. At this time, the patient is encouraged to take notes in the margins and ask questions. They are also told that they should take their PODS when seeing their family physician, pharmacist, or when accessing community services.

The successful implementation of PODS in the inpatient units of CAMH marks a huge step towards addressing the need for better patient information at discharge. As the PODS team at CAMH works towards refining the process, the next frontier for PODS at CAMH is clear. As Jamal states,
“I know there's an outpatient project coming. We need to really put our attention to outpatients because I think the majority of our patients are outpatients and we want to prevent them from getting admitted in the first place.”

The impact of PODS goes beyond helping clinicians better deliver care. Patients at CAMH also recognize the significant improvements PODS brings to the discharge process.
“I met with a patient who asked if she could speak to me about her discharge experiences at CAMH. She brought her discharge summary with her. It was about eight pages in six-point font with large gaps in space. There were lists of organizations where she could have gotten service that were nowhere near where she lived and not appropriate to her needs. And then we walked through the PODS and as I showed it to her, she teared up a bit at the idea that this could have been what she had received. PODS is now the rule, not the exception. It has become the norm and it's become a process that we abide by as part of every discharge.”
Thinking about implementing PODS for your patients? CAMH has three tips for you to get you on the right track:
CAMH’s Advice on Implementing PODS:
1) Make it about the patient experience: When we took the approach of saying “this is our response to what our patients are telling us in patient experience feedback” and not “this is what the literature shows” we received a lot more buy-in from our entire community.
2) Engage all key stakeholders, especially patients: As a part of the PODS implementation process, we consulted with many different stakeholders: patients, caregivers, physicians, nurses, therapists, family physicians, and community services to name a few. Doing so allowed us to catalogue the diverse needs and ensure that they were considered during implementation.
3) Use data to your advantage: CAMH is a data-driven institution and we used that to our advantage. By understanding our patient experience data, and cross-referencing it with the literature, we were able to pinpoint the need and track it throughout the project. We also created a dashboard that we used to show how PODS was positively impacting transitions in care to maintain support and engage our colleagues in a conversation about our discharge processes.